
16 Nov Menopause Matters: So Let’s Talk, Know and Do More About It
Written by Prabjit Chohan-Patel
SHE Malta is not qualified to offer medical advice nor proof of the efficacy of conventional or alternative treatments. This article should not be used to make any final decisions about perimenopause or menopause management or treatment. Its sole aim is to provide clarifications and information as a starting point for a consultation with your doctor to discuss the best route for you individually.
Today’s increased life expectancy means more women are living a third – even half – of their lives in a post menopausal state. As the SHE Malta community is made up of women who will either hit this life stage in the future or already have done so, we’re departing from our usual business-focused content and looking at this significant and inevitable health and life issue. An issue that the SHE Word host Trudy Kerr tellingly describes as “affect[ing] every single woman on the planet but the most un-talked about topic I think I have ever come across”. This is no exaggeration. Menopause and everything surrounding it seems to be the elephant in the room.
While we can’t cover this topic entirely, we will be addressing the main aspects in a three part series, starting with this article. Part 1 presents an overview of menopause, historically and sociologically and explains the biology of what happens to the female body and the consequent health implications. We’ll list the available options for symptom reduction and relief. Part 2 will look at HRT, the background, options, benefits and risks. Part 3 will address some common misconceptions about menopause and hopefully answer many of your own questions (including the ones you didn’t know you had!) in the hope of forging a path through the confusion.
Society…a brief history of menopause
Often referred to as “The Change”, menopause is a stage of life that all women – fortunate enough to reach a certain age – inevitably experience. While many things in life are a woman’s choice, menopause is not. It is unavoidable. The chain reaction it sets off is complex and goes way beyond the simplicity of its name (Greek: ‘meno’ = month, ‘pausis’ = cessation) and its impact on female health and quality of life is far-reaching and profound.
Yet for some reason, this significant health issue has often been misunderstood, misdiagnosed, overlooked or incorrectly treated. The hush hush taboo status that has been – and continues to be – attached to this part of a woman’s life has compounded the situation, resulting in generations of women feeling that menopause is an automatic life sentence of decay and deterioration to be simply endured in silence. In fact, some of us may recall it affecting our mothers/grandmothers/older sisters but not understanding what was ‘wrong’ with them.

Many societies have commonly viewed women going through this change as permanently depressed, crazy and written off as no longer useful (as if the physical and mental realities of menopause are not punishing enough). Vanessa Coleiro – brand consultant and natural health enthusiast – mentions that American women in the 1950’s were routinely told their menopausal symptoms were “in their head’ and that they were simply bored, attention-seeking housewives who should join the PTA!
Moira Delia, speaking on Trudy Kerr’s podcast admits people tended to react in shock when she mentioned she was in early menopause and also feels denial is a big issue.
It is also not inconceivable to suggest women (more so in certain parts of the world than others) are more likely to address the visible signs of midlife by going to a med-aesthetic practitioner for Botox, dermal fillers etc than they are to address the physical and mental aspect by going to a gynaecologist for HRT.
Menopause and Geography
The Western view of menopause as being something to be dreaded is vastly different from the one held by certain other cultures. The Japanese for instance appreciate this as a welcome transition towards renewal and regeneration. In New Zealand, traditional Maori culture respects middle aged women for the wisdom they can offer. And the Mayans value older women so greatly they place them at the very centre of their culture and community for the life experience they can teach future generations.
It’s worth noting that women’s symptoms vary according to country (lifestyle including diet could play a part in this). In her article “An Overview of Menopausal Disorders”, Dr Heidi Grech mentions that Japanese and Chinese women tend to suffer fewer symptoms than North American women.
Although we are beyond the decades-ago thinking mentioned earlier, menopause education and treatment has still not advanced to the level one might expect. And it seems to be a case of geographical lottery as the BBC also recently revealed. Depending on where one lives, the level of attention and support given to peri menopause management can vary greatly, either resulting in a woman feeling supported, well informed and able to make the right decisions for her health and quality of life. Or instead unaware, in physical discomfort, abandoned and helpless to take charge of her current and future medical safety.
A 2021 study conducted in the USA found 73% of women were not treating their menopausal symptoms and 45% of women didn’t know the difference between perimenopause and menopause.
On a positive note, many women themselves can feel liberated by no longer having to endure pain, weakness from blood loss, expenditure on sanitary products or limited activity due to monthly periods.
Awareness
The fact there is an entire month dedicated to menopause awareness each year perhaps bears proof of the incredibly common scenario that is emerging: many women themselves often fail to recognise what is happening to them or know what to do even when they have realised their body and health is changing negatively. The commentary I see on menopause forums, the interviews and research I’ve done (and indeed my personal experience) all confirm this.
As Yvonne Midolo, Podiatrist, says “Health literacy is not automatically connected to one’s intelligence”. Below are just a few of the discoveries I’ve made the last few years from talking to several friends across the UK, France, Germany and Malta:
-Many women revealed their difficulty in obtaining clear advice – some women ‘laughed out of’ their appointment by a dismissive doctor (in most cases male) unwilling to offer relief options to any woman under the age of 50.
-Conversely, three people in Malta said any ailment they mentioned to their GP was automatically associated with perimenopause with no discussion of other possible causes.
-Only two people – including myself – in their mid 50’s had done a bone density scan.
-Several of my friends have never seen a consultant or done independent research for HRT
-Hardly anyone had heard of perimenopause until their early 50’s (i.e. after it had finished)!
-Almost everyone was initially uncertain over which medical professional to see: general practitioner, gynaecologist, endocrinologist?
-Absolutely everyone said they no longer recognised themselves but couldn’t pinpoint when they started feeling this way.
On her podcast, Trudy admits she only discovered she was well into menopause after visiting a doctor regarding unexpected symptoms she was experiencing: “I had not prepared for it but of course, I’m 48 and you would expect that this might happen!,” she says, adding “I had never heard of perimenopause”.
Maybe it’s not so surprising then that Dr Olivia Anne Cassar, Malta-based gynaecologist, revealed that out of all her annual patients, only two visit her to discuss menopause (interestingly, these are usually expat, not Maltese patients).
What are the possible contributing factors?
-The inadequate infrastructure within many healthcare systems resulting in a lack of obvious, accessible and robust information on menopause – in stark contrast to the amount of information (depending on country) on other female health areas such as breast cancer screening, pregnancy and fertility, contraception, STD’s, cervical cancer screening etc.
-A tendency in many Western medical cultures to only deal with the mental aspect of menopause via antidepressants instead of adressing the other symptoms via HRT or supplements etc.
The frequent inability – and in many cases unwillingness – of partners or family to understand or provide support for their female partner’s/relative’s mental and physical state in midlife.
-The absence of guidelines or policies within the workplace to support female employees, a valuable and vital part of the economy – in menopause. (400k women resign annually in the UK due to the grave mental and physical impact of menopause – a huge amount of the workforce and skills force lost.)
Doctor, doctor.
In light of this, it is not that surprising that many general practitioners or family doctors are not well equipped to help patients in this area. Edinburgh GP Dr Maria, admits “Menopause is barely covered at medical school: the onus is really on individual general practitioners to ensure that they are up-to-date and knowledgable about current menopause management guidance, by paying to attend or study specific courses on the subject.”
In fact, a doctor I spoke to at a leading clinic in Malta admitted to feeling embarrassed at her lack of menopause knowledge. It also transpires that doctors only recommend synthetic HRT in Malta, despite there being a clinic offering customised bioidentical hormones.
So you could be forgiven for thinking menopause matters don’t…well…matter. But menopause is a hot (flush) issue…
So WHAT exactly are perimenopause, menopause and postmenopause?
In the bloom of life, the female body’s ovaries produce the key reproductive hormones oestrogen, progesterone and testosterone. Around ages 40-44 (on average), oestrogen levels decrease, throwing off the balance with progesterone. (Testosterone decrease is more a symptom of natural ageing rather than menopause.) This is perimenopause. As oestrogen and progesterone are both responsible for ovulation and menstruation, their decrease inevitably leads to unpredictable menstrual cycles. Perimenopausal hormone levels can resemble a rollercoaster, causing numerous symptoms including anxiety, mood swings, brain fog, hot flushes and increased sweating, all marking the transition towards the next stage.
Menopause (between ages 45-55, but most commonly 51 years) is defined as the point at which 12 months have passed since your last period. This is the stage where your body is making so little oestrogen that your ovaries stop releasing eggs altogether, causing the end of menstrual periods.
Once more than a year has passed after the last period, the body enters postmenopause. This stage defines the rest of a woman’s biological life, from which there is no return or further stage.
What does the female body experience?
The list of symptoms is long and the number and intensity of symptoms experienced varies between individuals. Some symptoms are short term and more prevalent in an individual stage eg perimenopause and other symptoms are connected to long term postmenopause health.
Physical:
Joint aches and stiffness (unrelated to previous illness or injury)
Weight gain
Increased sweatiness
Tension headaches due to hormonal changes
Low libido and pain from intercourse
Palpitations
Hot and cold flashes (most often together)
Night sweats
Osteopenia
Vaginal dryness (atrophy)/itching
Frequent urination
Incontinence
Increased fatigue
Hair loss: widening parting, receding hair line, thinning hair texture
Nail breakage and dry skin
Formication prickly skin sensation
Bleeding gums
Height shrinkage
Mental
Poor concentration (causing slower learning time) and brain fog
Confusion and less ability to think logically, plan simple tasks and make decisions
Memory loss (difficulty recalling everyday words, placement of items, names of people and places)
Clumsiness from impaired judgement of space and distance.
Emotional
Anxiety, overwhelm and nervousness
Feeling low and/or easily weepy.
Apathy, feeling directionless or uninterested in life, reclusiveness and withdrawing socially
Feeling invisible, loss of identity, self confidence, feminine self (also connected to physical sexual dysfunction above)
My menopause, your menopause.
No two women’s experiences are the same. Some women are lucky enough to pass through the various stages with mild symptoms and little physical discomfort while others suffer greatly, to the point where they can barely function. Chances are if you chat to a handful of friends, you’ll all have different stories and symptoms about the same natural physiological event!
Dr Olivia Anne confirms: “I have seen women who sail through these years without any problems and I have encountered patients who burst into tears in clinic as they cannot put on a spot of make up without it melting off their faces within the hour.”
A few things are certain: it is important to be aware of your symptoms in order to know what to do about them. And it is essential to be kind to yourself. Self care is not a nice-to-do but a must at this stage of life.
What options are available to relieve or minimise symptoms?
The adage prevention is better than cure couldn’t apply more and it is a good idea to take steps during the perimenopause years to increase your chances of a more comfortable menopause. Nevertheless, whatever stage of menopause you are at (peri, menopause transition or post menopause), it is not too late to tackle your symptoms as long as you do not leave it til many years after your last period. (Post menopause, if left unsupported, can have serious ramifications for long term health including osteoporosis, heart disease, osteoarthritis and dementia.)
Many women wish to address this stage in life as naturally as possible, without pharmaceutical intervention. This requires a ‘whole life style’ approach including the aid of:
– exercise – cardiovascular, weight-bearing, yoga, pilates
– consistent sleep schedule and sufficient rest
– diet high in proteins, vegetables and food groups that are low on the glycaemic index
– low to moderate alcohol consumption
– mindfulness – meditation
– acupuncture
– massage – abhyangha (Aryuvedic), aromatherapy and Swedish
– supplements
Interestingly, Vanessa Coleiro, Brand Consultant and Natural Health Enthusiast, has spent time studying the connection between liver and colon health and the endocrine system, discovering that menopausal hormonal imbalance is potentially worsened by a clogged up liver and colon. A big believer in the new generation of plant-based detox and power nutrition programmes, Coleiro is convinced that cleansing the liver and colon – thereby supporting the endocrine system – greatly reduces and even eliminates many significant symptoms including weight gain, hot flushes and poor sleep.
Supplement Me
The potential use of supplements for menopause is worthy of an article in itself (or even its own three part series!). Evening primrose oil, curcumin, moringa, turmeric, collagen, Vitamin D, calcium, red clover, black cohosh, Flaxseeds, Ginseng, Valerian have been shown to deliver benefit (to different degrees) when used with an understanding of dosage and potential side effects.
In addition, an increasing number of menopause-specific supplements are hitting the market, designed for those women not wishing to go down the ‘pharmaceutical HRT’ route. Companies such as Happy Mammoth and Better Body are tackling some of the most common symptoms such as the midlife tyre, hair loss and fatigue with a range of different products including Bloat Banisher and Provitalise. Biocare and Vitabiotics have been offering their own ‘complete menopause’ supplements for years.
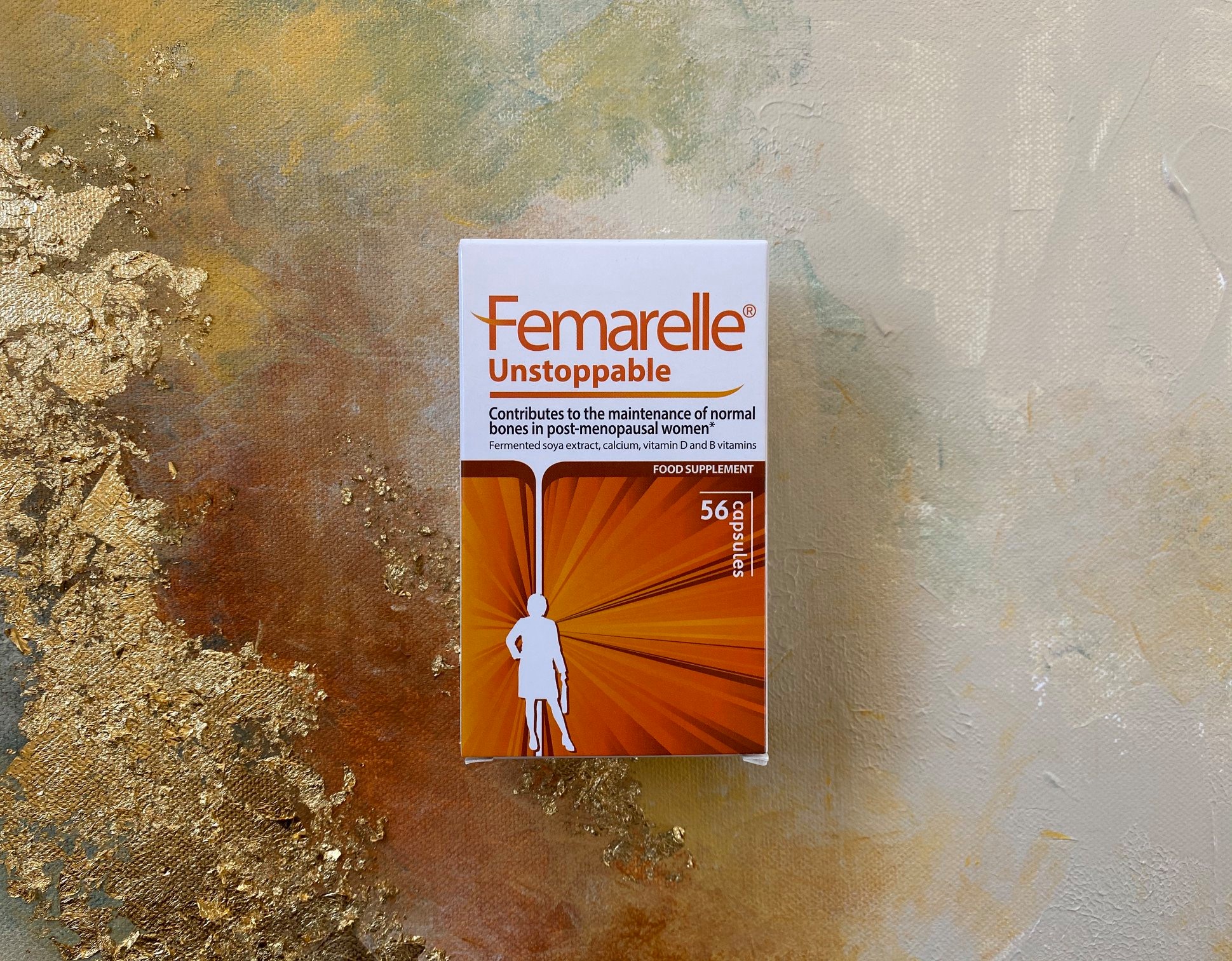
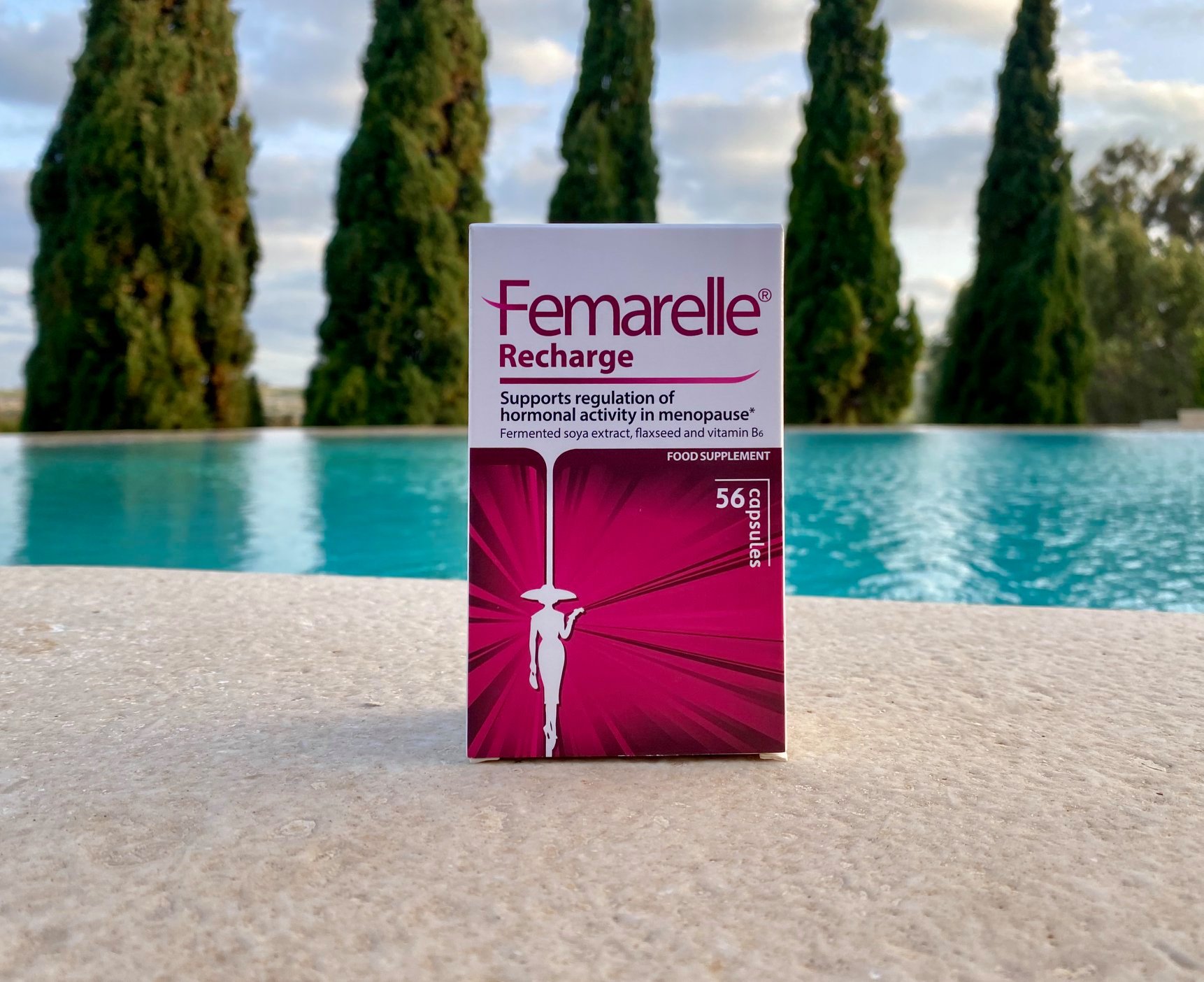
Meanwhile, Femarelle® is another leading provider of menopause-focused supplements. Available in several territories worldwide, the Femarelle® range consists of three different lines designed to support different stages of the menopausal journey: Rejuvenate, Recharge and Unstoppable. We’ll be taking a closer look at how the Femarelle® products work in Part 2 of our Menopause Matters series.
HRT
Today, HRT is credited as being the most effective way of relieving the most common menopause symptoms and reducing the risk of osteoporosis and dementia. Combined HRT – oestrogen and progesterone – can either be taken in separate forms or both hormones are combined in one preparation called progestogen. Different factors influence what is prescribed for the patient. Oestrogen-only HRT is only for women who have had a hysterectomy.
HRT is available in three forms:
– traditional ‘classic’ synthetic (chemically produced and not identical to human hormones, sometimes the only form available in a country)
– body identical HRT (increasingly preferred, considered by medical professional as safest and available in many countries)
– bio identical (less commonly available depending on where you live and currently not FDA approved).
HRT can be taken in numerous ways such as oral tablets, sprays, dermal patches, creams, gels, vaginal pessaries and intrauterine coil, depending on the symptoms, medical history and needs of the patient. Not all methods are available in all countries or available in bioidentical HRT form. We’ll be delving into HRT more in Part 2 of our Menopause Matters series.
Let’s turn the tide.
Awareness campaigns are being seen in certain countries. Known media personalities such as Davina McCall are publishing books on menopause and raising an immense amount of publicity about the daily struggle of women in menopause. Conversations are happening aimed at destigmatising menopause. Gynaecologists are also more willing to prescribe HRT as treatment. It’s a step in the right direction.
As Dr Oliva Anne puts it: “Patients are also more aware that menopause is not something they have to endure but rather something they have to live through with a positive attitude. I feel this shift in mentality is a healthy one and I look forward to seeing it improve further in the coming years as I approach my own!”
DON’T MISS PART 2: “To HRT or not to HRT?”











Sorry, the comment form is closed at this time.